A chocolate cyst, often linked to endometriosis, is a noncancerous ovarian cyst filled with dark brown fluid that resembles old menstrual blood. It affects 20-40% of women with endometriosis and can cause chronic pelvic pain, painful periods, and even infertility. These cysts form when endometrial tissue grows outside the uterus. Understanding their symptoms, causes, and treatment options is essential for managing your health. If you want to learn more about these cysts, there's much more to explore!
Key Takeaways
- A chocolate cyst is a noncancerous ovarian cyst filled with old menstrual blood, often linked to endometriosis.
- These cysts typically cause chronic pelvic pain, especially during menstruation, and can lead to infertility issues.
- Diagnosis involves imaging techniques like transvaginal ultrasound and MRI to assess cyst size and characteristics.
- Treatment options range from hormonal therapies to surgical removal, depending on cyst size and symptoms.
- Regular monitoring and personalized care are essential for managing symptoms and maintaining reproductive health.
What Is a Chocolate Cyst?

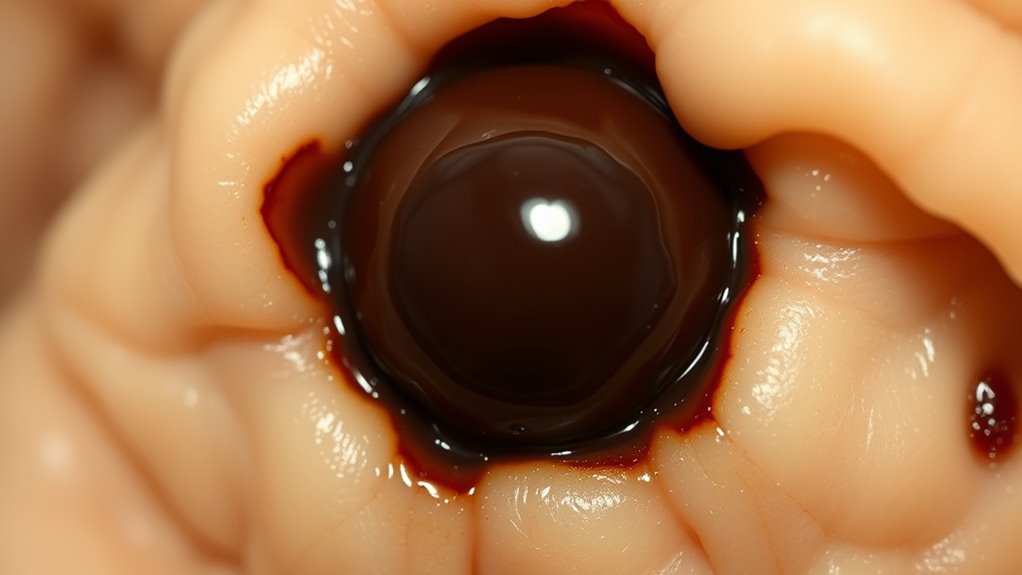
A chocolate cyst, or ovarian endometrioma, is a type of noncancerous cyst that forms in the ovaries, primarily in women with endometriosis.
These cysts develop from endometrial tissue that grows outside the uterus, often filled with old menstrual blood, giving them a dark brown appearance. Interestingly, pet therapy has been shown to enhance emotional well-being, which may benefit women coping with the stress of such health issues. Additionally, the emotional impact of trust issues may complicate the experiences of women dealing with both endometriosis and chocolate cysts. Maintaining a positive mindset is essential for coping with the challenges of wilderness survival. Furthermore, proper planning and awareness of health conditions can help women manage their overall well-being and maximize benefits during treatment.
Chocolate cysts form from endometrial tissue outside the uterus, often containing old menstrual blood, resulting in their characteristic dark brown color.
Curiously, around 20 to 40 percent of women with endometriosis may experience chocolate cysts.
While symptoms can include pelvic pain and painful periods, the size of the cyst doesn't always indicate symptom severity.
Diagnosis typically involves a pelvic ultrasound, and a definitive diagnosis may require fluid extraction for testing.
Treatment options range from watchful waiting for small, asymptomatic cysts to surgical removal for larger or painful ones, allowing many women to conceive naturally despite having chocolate cysts. Additionally, the emotional and psychological effects of dealing with narcissistic abuse can complicate recovery for women facing health issues like chocolate cysts.
Symptoms of Chocolate Cysts

Many women with chocolate cysts experience chronic pelvic pain, especially during their menstrual cycles. This pain can be debilitating and often worsens with dysmenorrhea, characterized by crampy periods. Additionally, it's important to note that hormonal imbalances can exacerbate these symptoms. Regular check-ups can also help monitor cold medications that may interact with other treatments. Early intervention can be beneficial, as palliative care options can provide support in managing chronic pain. Moreover, understanding the importance of advance directives can help guide healthcare decisions if complications arise.
You might also face other symptoms that indicate the presence of chocolate cysts:
- Dysmenorrhea (painful menstrual periods)
- Dyspareunia (pain during sexual intercourse)
- Infertility, often linked to severe endometriosis
- Sudden and severe abdominal pain, which may indicate a rupture
- General discomfort in the pelvic region
If you're experiencing these symptoms, it's crucial to consult a healthcare provider. Mammography guidelines recommend early detection methods to help manage health concerns effectively.
Addressing chocolate cysts early can help manage pain and reduce complications related to endometriosis and potential infertility.
Causes of Chocolate Cysts

Understanding the causes of chocolate cysts is essential for managing your reproductive health.
These cysts often stem from endometriosis, where tissue similar to the uterine lining grows outside the uterus, influenced by hormonal changes and various genetic or environmental factors.
Endometriosis Role Explained
Although chocolate cysts are often associated with endometriosis, their formation is a direct result of endometrial-like tissue growing outside the uterus. This tissue can attach to your ovaries, leading to ovarian endometriomas filled with old blood during your menstrual cycle.
Hormonal changes, especially during ovulation, may trigger bleeding into these cysts, causing increased pain and inflammation.
Here are some key points about the role of endometriosis in chocolate cysts:
- Endometrial tissue grows outside the uterus.
- Cysts form during your menstrual cycle.
- Symptoms can include severe pain.
- Risk factors include family history and early menstruation.
- Hormonal changes can exacerbate the condition.
Understanding these aspects can help you identify and manage chocolate cysts more effectively.
Hormonal Influences on Formation
Hormonal fluctuations greatly influence the formation of chocolate cysts, also known as ovarian endometriomas. These cysts develop from endometrial-like tissue that responds to hormonal changes during your menstrual cycle.
Estrogen and progesterone stimulate this tissue, causing it to proliferate and bleed, which results in the accumulation of old blood and the cyst's characteristic chocolate appearance. During ovulation, hormonal changes can lead to additional bleeding within the cyst, intensifying inflammation and pain.
Increased estrogen levels are particularly significant, as they promote the growth of endometrial tissue outside the uterus. Consequently, the cyclic nature of these hormonal shifts can lead to chronic inflammation and painful periods, making the experience of living with chocolate cysts more challenging.
Genetic and Environmental Factors
Genetic and environmental factors greatly contribute to the development of chocolate cysts, making it essential to take into account both when evaluating your risk. Understanding these influences can help you identify potential risk factors, including:
- Genetic predisposition: A family history of endometriosis increases your chances of developing chocolate cysts.
- Environmental factors: Exposure to endocrine-disrupting chemicals might elevate risk.
- Retrograde menstruation: When menstrual blood flows backward, it can lead to endometriosis and cysts.
- Hormonal imbalances: Higher estrogen levels can promote the growth of endometrial-like tissue on your ovaries.
- Menstrual cycle abnormalities: Early onset of menstruation may also be a contributing factor.
Recognizing these elements is vital for proactive health management.
Diagnosis of Chocolate Cysts

When diagnosing chocolate cysts, imaging techniques like pelvic ultrasounds play an essential role in spotting cysts.
However, to confirm the diagnosis, a needle biopsy may be necessary for a closer look at the cyst's fluid.
Understanding these steps helps guarantee accurate identification and management of the condition.
Imaging Techniques Used
Imaging techniques play an essential role in diagnosing chocolate cysts, as they help visualize these cysts' size and location. You might encounter various methods, each serving a unique purpose:
- Transvaginal ultrasound: Effective for identifying ovarian endometriomas, showcasing a "ground-glass" appearance.
- Ultrasound: Commonly used to detect chocolate cysts and assess their dimensions.
- MRI: Helpful for evaluating complex cysts and determining the extent of endometriosis beyond the ovaries.
- Needle biopsy: Guided by ultrasound, it allows for fluid extraction to confirm the diagnosis.
- Follow-up ultrasounds: Necessary to monitor changes in cyst size or symptoms over time.
These imaging techniques are vital in ensuring accurate diagnosis and appropriate management of chocolate cysts.
Confirmatory Tissue Analysis
Confirmatory tissue analysis is essential for accurately diagnosing chocolate cysts, as it provides definitive evidence that distinguishes them from other ovarian cysts.
Typically, this involves a needle biopsy where fluid is extracted from the cyst under ultrasound guidance for microscopic examination. While ultrasound can identify cysts, it can't definitively determine their type without further analysis.
The extracted fluid from a chocolate cyst often reveals characteristics consistent with old blood, confirming its identity as an endometrioma. This diagnosis is significant for differentiating chocolate cysts from other ovarian cysts, which may require different treatment options.
Accurate tissue analysis is critical, especially when fertility is a concern, ensuring you receive the most appropriate management for your situation.
Treatment Options for Chocolate Cysts
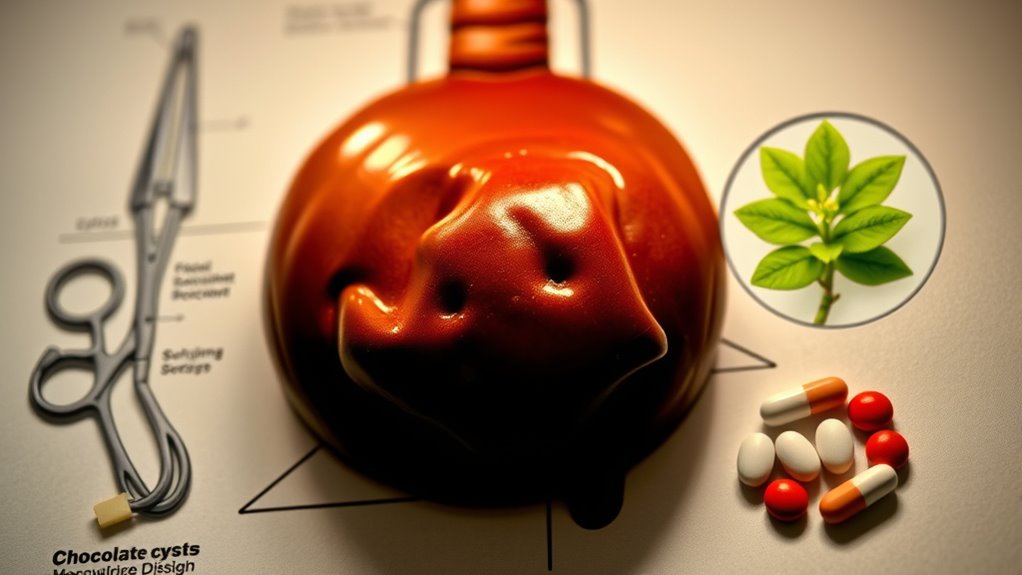
While chocolate cysts can be a source of discomfort and concern, treatment options are tailored to your specific situation, including the cyst's size, symptom severity, and your reproductive goals.
Chocolate cysts can cause discomfort, but treatment is personalized based on size, symptoms, and reproductive goals.
Here are some common treatment options:
- Observation for small, asymptomatic cysts
- Hormonal treatments like the Mirena IUD or birth control pills to manage symptoms
- Laparoscopic surgery for symptomatic chocolate cysts, preserving healthy ovarian function
- Surgical removal to alleviate pain and improve fertility rates, particularly for those with endometriosis
- Follow-up care to monitor recurrence and overall reproductive health
Each option aims to address your unique needs and enhance your quality of life while managing the presence of chocolate cysts.
Impact on Fertility and Outlook

Understanding the impact of chocolate cysts on fertility is vital for women managing their reproductive health. These ovarian endometriomas can cause inflammation and scarring, hindering the implantation of fertilized eggs.
Approximately 30-50% of women with endometriosis experience infertility, highlighting the need for monitoring symptoms related to chocolate cysts. Surgical treatment can greatly improve fertility rates, with success rates jumping to 85% for women seeking to conceive.
While some may conceive naturally, others might need assisted reproductive technologies like IVF, which show comparable success rates to other infertility issues.
Regular monitoring and timely treatment of chocolate cysts are essential, as persistent symptoms can severely affect your overall reproductive health and future fertility prospects.
Frequently Asked Questions
What Is the Main Cause of Chocolate Cyst?
The main cause of chocolate cysts is endometriosis, where tissue similar to the uterine lining grows outside the uterus and attaches to the ovaries.
This tissue can bleed during your menstrual cycle, leading to the formation of cysts filled with old blood, which gives them a chocolate-like appearance.
Hormonal changes and factors like retrograde menstruation may contribute to their development, though the exact mechanisms aren't fully understood.
What Size Chocolate Cyst Requires Surgery?
When it comes to chocolate cysts, you should consider surgery if the cyst is larger than 4 cm, especially if it causes you significant pain or discomfort.
Even smaller cysts can necessitate surgery if they're symptomatic. If you notice a rapid growth or unusual characteristics through imaging, a surgical evaluation might be needed, regardless of size.
Laparoscopic surgery is often the preferred method due to its minimally invasive nature and quicker recovery time.
What Happens if Chocolate Cyst Is Not Removed?
If you ignore a chocolate cyst, you're playing with fire. It can grow, causing increasing pelvic pain and discomfort.
Left untreated, it might lead to complications like infertility due to scar tissue blocking your fallopian tubes. There's also a risk of rupture, which can result in severe abdominal pain and internal bleeding.
Plus, persistent cysts can damage surrounding ovarian tissue and potentially heighten the risk of developing ovarian cancer, especially with advanced endometriosis.
How Long Does It Take for a Chocolate Cyst to Go Away?
If you're dealing with a chocolate cyst, it may resolve on its own within 4 to 8 weeks if it's functional and asymptomatic.
However, larger or symptomatic cysts usually won't go away without intervention. You might consider hormonal treatments, like birth control pills, which can help manage symptoms and potentially reduce the cyst size over time.
Regular monitoring through ultrasounds might be necessary to track any changes in size or symptoms.
Conclusion
In the journey through life, discovering a chocolate cyst can feel like stumbling upon a hidden obstacle. But remember, you're not alone in this. With the right diagnosis and treatment, you can navigate these murky waters and emerge stronger. Picture yourself basking in the sunlight again, free from the shadows of pain and uncertainty. Embrace the support around you, and take charge of your health—your future is bright and filled with possibilities.