Ovarian reserve refers to the total quantity and quality of eggs in your ovaries, and it declines markedly as you age, especially after 35. At birth, you have around 2 million eggs, but this drops dramatically over time. Evaluating ovarian reserve is essential for understanding your fertility, as diminished reserve can lead to challenges in conception. Curious about how it's measured and what it means for your fertility? There's much more to explore on this topic!
Key Takeaways
- Ovarian reserve refers to the quantity and quality of a woman's oocytes, influencing fertility potential.
- Women are born with around 2 million primordial follicles, decreasing significantly by age 35.
- Diminished Ovarian Reserve (DOR) affects conception chances and is linked to age and egg quality.
- Key tests for assessing ovarian reserve include AMH, FSH, and Antral Follicle Count (AFC).
- Regular monitoring and consultation with a fertility specialist are crucial for those over 35 trying to conceive.
Understanding Ovarian Reserve
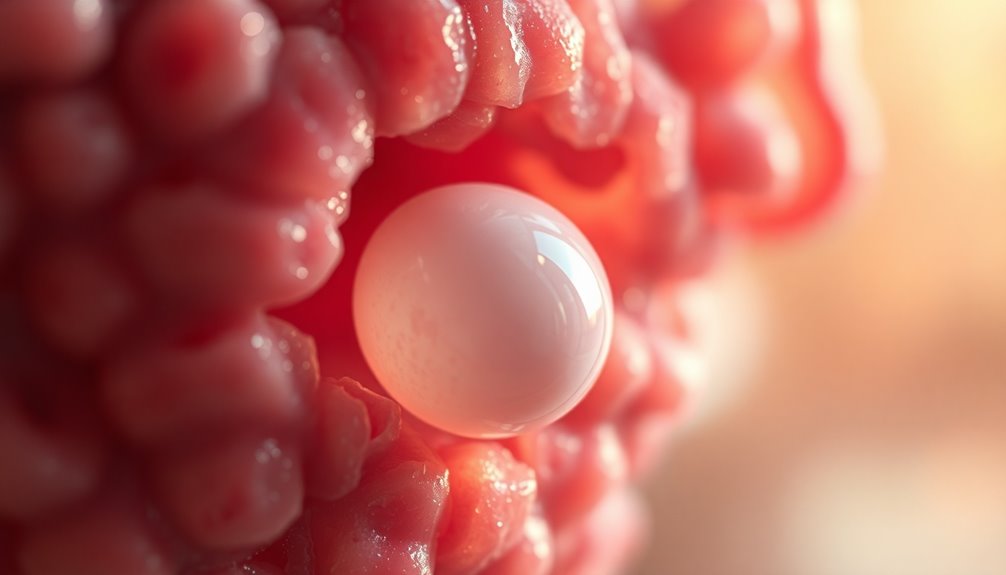
Understanding ovarian reserve is essential, especially as you age and consider your reproductive options. Ovarian reserve refers to the total quantity and quality of oocytes remaining in your ovaries, which decreases considerably after age 35.
At birth, you have about 2 million primordial follicles, but by your late 30s, this number dwindles to around 25,000. Diminished Ovarian Reserve (DOR) occurs when you have fewer eggs than expected for your age, affecting your response to fertility treatments and chances of conception.
Key factors like age, genetics, and environmental exposures influence your ovarian reserve. Testing methods, including Anti-Müllerian Hormone (AMH) levels and Antral Follicle Count (AFC), provide insights into your reproductive potential and egg quality, guiding your menstrual cycles and fertility journey. Additionally, understanding the importance of awareness about reproductive health can empower you to make informed decisions regarding your fertility.
Importance of Ovarian Reserve Testing

Ovarian reserve testing plays an essential role in evaluating your reproductive health and fertility potential. By measuring key indicators like Anti-Müllerian Hormone (AMH), Follicle Stimulating Hormone (FSH), and Antral Follicle Count (AFC), you gain valuable insights into your egg quantity and quality.
These assessments are vital, especially when considering assisted reproductive technologies like IVF, as they predict your response to fertility treatments. Regular monitoring of your ovarian reserve becomes increasingly important as you age, particularly after 35, when egg quality and quantity often decline. Additionally, understanding factors such as mammography guidelines can provide insights into how age-related changes might affect your overall health and reproductive decisions.
Understanding your ovarian reserve empowers you to make informed decisions regarding family planning and fertility preservation, guiding your reproductive journey with confidence and clarity.
Factors Affecting Ovarian Reserve

As you age, your ovarian reserve naturally declines, especially after your mid-30s. Lifestyle choices and environmental factors, like smoking and exposure to radiation, can also influence your egg quantity and quality. Understanding these factors can help you make informed decisions about your reproductive health. Additionally, monitoring your ovarian reserve through medical evaluations can provide valuable insights into your fertility.
Age Impact on Reserve
While many factors influence a woman's ovarian reserve, age remains the most significant. As you age, there's a notable decline in ovarian reserve, especially after 35.
You're born with about 2 million oocytes, but this shrinks to around 400,000 by menarche and drops to roughly 1,000 by menopause. The age impact accelerates after your mid-30s, affecting both the quantity and quality of oocytes, which can diminish your fertility potential.
Furthermore, genetic predisposition and environmental exposures, like smoking, can further exacerbate this decline. Diminished ovarian reserve (DOR) mightn't show symptoms, often being noticed only when seeking fertility help. Nutrition plays a crucial role in overall health, which could further influence reproductive functions.
Regular monitoring is essential to understand your reproductive lifespan and address any concerns early.
Lifestyle and Environmental Factors
When reflecting on factors that affect your ovarian reserve, lifestyle choices and environmental exposures play an essential role.
Smoking is a major lifestyle factor that can diminish your egg quantity and quality, making it harder to conceive.
Additionally, obesity can negatively influence ovarian reserve, as higher body mass index (BMI) often correlates with lower levels of anti-Müllerian hormone (AMH), a key marker of ovarian function.
Environmental exposures to radiation and harmful chemicals can also accelerate the loss of oocytes.
Genetic factors further complicate the picture, as inherited traits may predispose some women to diminished ovarian reserve earlier in life.
For a thorough fertility evaluation, it's important to reflect on how these influences impact your reproductive health. Understanding the concept of budget management can also help in planning financially for fertility treatments and related expenses.
How Ovarian Reserve Is Measured

When it comes to measuring your ovarian reserve, three key tests come into play: Anti-Müllerian Hormone (AMH) levels, Antral Follicle Count (AFC), and Follicle Stimulating Hormone (FSH) levels. Each test offers unique insights into your egg quantity and quality, helping you understand your reproductive potential. Additionally, understanding your reproductive health is crucial for making informed decisions about family planning.
Key Measurement Tests
Ovarian reserve is evaluated through several key measurement tests that provide insight into a woman's reproductive potential.
One of the main tests is the Anti-Müllerian Hormone (AMH) test, which measures hormone levels indicative of small follicles in the ovaries and can be taken anytime during your menstrual cycle.
The Antral Follicle Count (AFC), performed via transvaginal ultrasound, counts visible follicles and is typically done in the first four days of your cycle to predict ovarian response to stimulation.
Additionally, Follicle Stimulating Hormone (FSH) levels are checked around day 3; elevated FSH suggests low ovarian reserve.
While these tests help in evaluating ovarian reserve, no single test is considered a gold standard for determining your reproductive age and overall fertility treatment success. Understanding emotional well-being is also crucial, as it impacts overall health during the fertility journey.
Interpreting Test Results
Understanding how to interpret test results is key to evaluating your ovarian reserve accurately. Tests like AMH levels, FSH levels, and Antral Follicle Count (AFC) provide insights into your egg quantity and quality.
AMH levels remain stable throughout your cycle and predict ovarian response in reproductive technology, while FSH levels assessed on day 3 indicate low ovarian reserve if elevated.
The AFC measures visible antral follicles via ultrasound, reflecting your recruitable egg population. Additionally, understanding the emotional dysregulation associated with various mental health conditions can provide context for the stress that fertility challenges may impose.
Impact of Diminished Ovarian Reserve on Fertility

Diminished ovarian reserve (DOR) can considerably affect your fertility potential, especially as you age.
With DOR, you may notice increased levels of follicle-stimulating hormone (FSH) and decreased anti-Müllerian hormone (AMH), indicating a reduced response to ovarian stimulation during fertility treatments.
Increased FSH and decreased AMH levels signal diminished ovarian reserve, leading to lower responsiveness in fertility treatments.
As DOR progresses, the likelihood of successful conception declines, particularly for women over 35, where egg quality deteriorates. This decline raises the risk of chromosomal abnormalities and miscarriage.
DOR accounts for 20-25% of infertility cases, impacting approximately 15% of the population.
Factors such as age, genetic predisposition, and lifestyle choices like smoking can also negatively influence your reproductive potential, affecting both the quantity and quality of your eggs. Understanding how emotional instability can affect relationships during fertility challenges is crucial for maintaining support systems.
Risks and Limitations of Ovarian Reserve Testing

While ovarian reserve testing can provide valuable insights into your reproductive health, it's important to recognize its limitations and risks. Tests like AMH and FSH can help evaluate your ovarian reserve, but they don't assess egg health or guarantee successful fertilization. The accuracy of these tests varies depending on methods and laboratory standards, leading to different normal ranges.
| Testing Method | Key Considerations |
|---|---|
| AMH | Doesn't predict egg quality |
| FSH | Results can fluctuate |
| AFC | May not reflect overall fertility |
Even with normal ovarian reserve results, infertility can still occur due to unrelated factors. Regular monitoring is essential, as fertility can change, especially with age. Additionally, understanding the production quantity variance can help in planning future fertility treatments more effectively.
Next Steps for Individuals Considering Testing

What steps should you take if you're considering ovarian reserve testing?
First, consult a fertility specialist if you're over 35 and have been trying to conceive for six months, or after a year if you're younger. Discuss your personal circumstances and any concerns about infertility or reproductive health.
Regular gynecological visits are essential for monitoring your overall reproductive health and can include conversations about your menstrual cycle and family history of infertility.
Ovarian reserve testing can provide vital insights, especially for those with diminished ovarian reserve (DOR), helping guide your options for assisted reproductive technologies like IVF.
Frequently Asked Questions
What Does Your Ovarian Reserve Tell You?
Your ovarian reserve gives you crucial insights into your fertility potential.
It reflects the quantity and quality of your remaining eggs, which naturally decline with age. Testing measures hormone levels and follicle counts, helping you understand your chances of conceiving naturally or through assisted reproductive technologies.
If you're considering delaying pregnancy or exploring fertility treatments, knowing your ovarian reserve can guide your decisions and help you plan effectively for your reproductive future.
What Is the Ovarian Reserve?
Have you ever wondered what happens to your eggs as you age?
Ovarian reserve is the term that describes the quantity and quality of your remaining oocytes. It starts high at birth but decreases over time, especially after age 35.
By then, you might find fewer eggs available, impacting your fertility.
Key markers like Anti-Müllerian Hormone (AMH) and Antral Follicle Count (AFC) help assess how your ovarian reserve changes throughout your life.
What Is a Normal Ovarian Reserve Level?
A normal ovarian reserve level varies with age.
For instance, at age 25, you'd expect an Anti-Müllerian Hormone (AMH) level around 3.0 ng/mL, while by age 45, it could drop to about 0.5 ng/mL.
Follicle Stimulating Hormone (FSH) should be below 10 mIU/mL on day 3 of your cycle, and an Antral Follicle Count (AFC) of 10-15 follicles is considered normal.
These factors indicate your fertility potential.
What Test Shows Diminished Ovarian Reserve?
To determine if you have diminished ovarian reserve, you'll want to look at specific tests. Elevated follicle-stimulating hormone (FSH) levels, typically over 10 mIU/mL on day 3 of your cycle, can indicate low ovarian function.
Additionally, low anti-Müllerian hormone (AMH) levels, generally below 1.0 ng/mL, suggest a poor response to fertility treatments.
Finally, a reduced antral follicle count (AFC) of fewer than 5-7 follicles also points to diminished reserve.
Conclusion
In understanding ovarian reserve, you empower yourself with knowledge; in testing your reserve, you take control of your fertility journey; in recognizing the factors at play, you embrace your unique health story. Whether you're seeking answers or considering next steps, remember that awareness leads to informed choices. So, stay curious, stay proactive, and stay hopeful. Your path to understanding and managing your reproductive health starts now, and it's a journey worth taking.









